Premature infants that are born prior to 34 weeks of gestation (6 weeks before their due date) or born less than 2000 grams at birth, are at increased risk of developing various health complications when compared to infants that are born full-term (37-40weeks of gestation). One such risk is Retinopathy of Prematurity (ROP), a disorder of the developing retinal blood vessels in the eye. ROP is the leading cause of childhood blindness in premature babies that are born too soon or those with low birth weight. In India, babies who are born less than 2000 grams (2 kgs) or 6 weeks before their due date (34 weeks of gestation) are at higher risk of developing ROP.
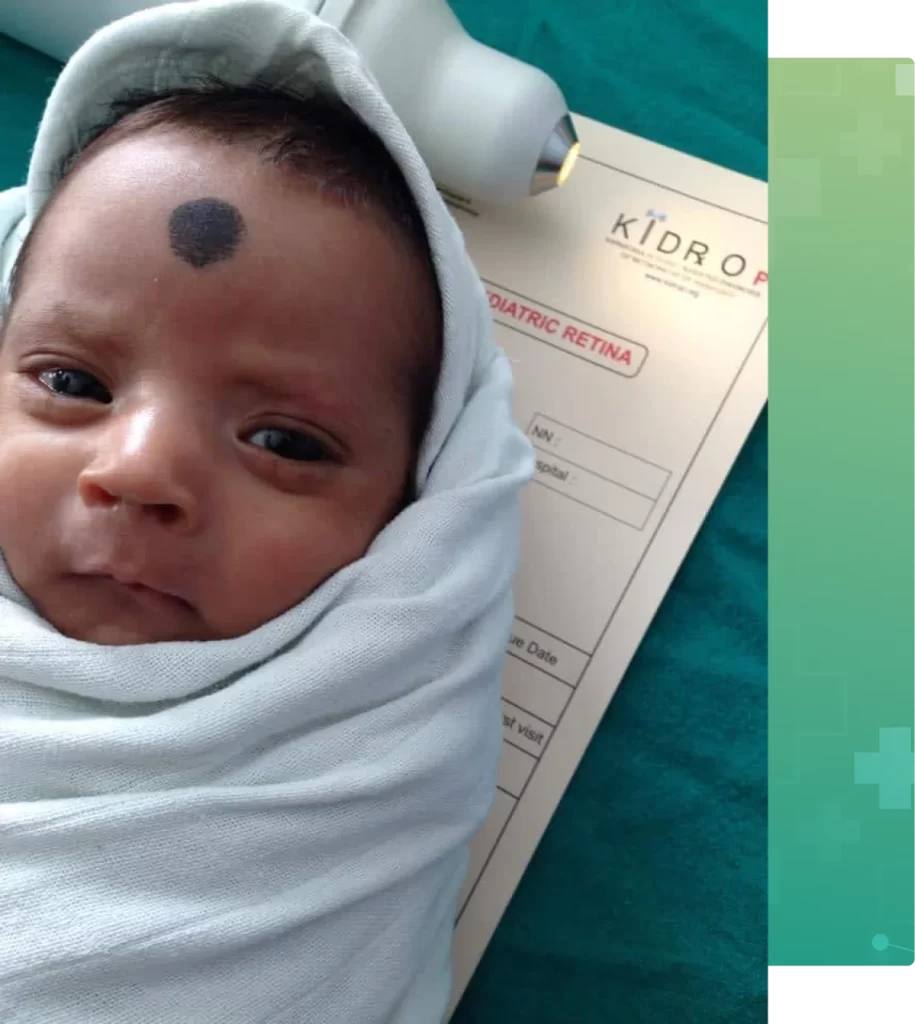
Karnataka Internet Assisted Diagnosis for Retinopathy of Prematurity (KIDROP) is Narayana Nethralaya’s flagship tele-ROP program started in 2007. KIDROP is a tele-medicine platform that benefits preterm babies born in neonatal intensive care units (NICUs) who do not have an ROP specialist to screen and treat the babies on time. Mobile teams of trained imagers use specialized ROP cameras to take images of the baby’s retina and upload it on the platform to be graded by Narayana Nethralaya’s ROP team. The Indian National ROP guidelines (2018) formally allowed imaging as the alternative method for ROP screening.

KIDROP was India’s first tele-ROP program and is currently one of the largest single-centre ROP programs in the world. In all, (by 2024), 177 NICUs across the state of Karnataka (Government and Private) are covered each week. Over 321,000 screening sessions have been completed and over 5200 babies treated thus far. This program is a public-private partnership with the Government of Karnataka and has mentored other ROP programs across the country. KIDROP has received several awards nationally and internationally for its innovations, including Public-Private Partnership of the Year in 2012, National Award for Excellence in HealthCare in 2016, K R Datta Award for Community Outreach in 2017, and BIRAC Innovator Award for HealthCare in 2018.
Narayana Nethralaya is equipped to perform ROP treatments of all forms with ease in new-borns and young children thanks to a dedicated, state of art Paediatric eye surgery operating room. We are the first centre in India to use OCT imaging to monitor infants for ROP and vision development – including CVI, retinal dystrophy and poor vision. Our ROP specialists care for hundreds of infants with ROP each year and will discuss your child’s treatment options in detail with you.

The two biggest risk factors for developing ROP are premature birth and a low birth weight (most common in 11% – 56% of preterm infants with low birth weight). A baby’s eyes develop the most during the last 3 months of pregnancy in the womb. When a baby is born early, the development of the retina is incomplete and there is a risk that the blood vessels which supply oxygen to the eye may not grow normally, which can lead to ROP.
Other than premature birth and low birth weight, many other factors can place these babies at higher risk of ROP. This includes prolonged use of oxygen, sepsis (blood infection), blood transfusion, jaundice, low weight gain, low platelets, anaemia (low haemoglobin), intraventricular haemorrhage (bleeding in the brain), etc.
If your baby was born premature, you may have concerns about ROP affecting your child’s vision. Narayana Nethralaya recommends an ROP screening a few weeks after delivery (first screening before 30 days after birth or earlier) for premature babies and babies that weigh less than 2 kgs at birth, and before they are discharged from the hospital. Timely diagnosis and early treatment can improve the chances of preserving vision.

The retina is responsible for one’s vision and any damage to it can lead to vision loss or blindness. Sadly, there are no visible signs of ROP externally when it first develops in a new-born. As a result, many parents do not get their babies screened on time. In advanced stages of ROP, there is a white reflex (leukocoria) in the centre of the pupil (round black portion of the eye). Unfortunately, by the time there are signs (when the baby is 4 – 6 weeks old) it is too late to save useful vision. An untreated infant with advanced ROP will have poor vision, poor eye contact with the parent, abnormal shaking of the eyes (nystagmus), and often delayed milestones as well.
Subtle changes in a baby’s retina can only be detected by a Paediatric retinal (ROP) specialist during an eye test where the baby’s retina is examined using special instruments. Narayana Nethralaya recommends an ROP screening for all preterm infants shortly after birth and once again before they go home from the hospital. Our paediatric retina team is trained to detect ROP before it becomes severe enough to result in retinal detachment.
The severity of ROP is graded into stages, from stage 1 to stage 5, with stage 1 being the mildest and stage 5 the most severe.
Another form of severe ROP is the ‘Aggressive ROP’ (called AROP) where stages 1 to 3 are skipped and it goes directly to stages 4 and 5. These cases are the most difficult to diagnose and treat.
The Paediatric retina department at Narayana Nethralaya offers therapeutic intervention for all stages of retinopathy of prematurity (ROP) which include, digital retinal imaging, OCT evaluation of retinal vasculature, fundus angiography for vessel and disease monitoring, laser treatment, anti VEGF injections for severe ROP and retinal surgery for the advanced ROP stages. Our team is trained to identify ROP in preterm babies and will recommend the proper treatment to ensure that the baby’s vision is safeguarded.
The purpose of ROP screening in premature infants is early detection of the condition so that it can be treated effectively to prevent vision loss. Doctors cannot predict which preterm baby will develop ROP as there are no visible signs or symptoms of the condition in the early stages, therefore screening is crucial. In India, the national ROP guidelines (2018) recommend that all babies born less than 2000 grams and/or premature (less than 34 weeks of gestation), must undergo their first ROP screening before they are 30 days old.
All premature infants should be monitored for ROP even after discharge from the hospital, as the condition is not always evident immediately after birth. Special wide field retinal imaging equipment is used by our team to screen the premature infant either in the NICU at the maternity hospital or at our hospital if the baby has already been discharged. If any signs of ROP are present, our ROP specialists will schedule follow-up exams to monitor the baby’s condition and determine when treatment is needed.

ROP needs to be diagnosed by an ophthalmologist who is trained in ROP management. The Paediatric Retina department at Narayana Nethralaya is equipped with the most up-to-date technology to detect ROP in preterm infants. Our Pediatric retina and ROP specialists are trained in the diagnosis of ROP and will carefully examine the inside of your preterm infant’s eyes for any abnormalities in the retina. The examination only takes a couple of minutes and will not hurt the baby.Eye drops are used to dilate (enlarge) the baby’s pupils so that the retina can be studied. A specially designed eyelid speculum is used to hold the eyelids open. A viewing instrument called an indirect ophthalmoscope, which has a special lens that sends a bright light into the eye, is used by the specialist to examine the retina and retinal blood vessels. Additionally, a special camera such as a RetCam or Neo is used to take high-resolution digital pictures of the retina. This provides detailed images that help in the follow-up of the progress of the baby’s condition over time.
Here is what you can expect
If any signs of ROP are detected, the doctor will discuss the follow-up evaluations and treatment options with you.


Treatment will depend on the stage and severity of ROP. In most babies, ROP is mild and resolves on its own without treatment, causing no damage. However, infants with more severe forms of ROP will require treatment to reduce the chances of retinal detachment and permanent vision loss or blindness. ROP that requires treatment is called ‘Type 1 ROP’ and must be ideally treated within 48 hours of the diagnosis for the best outcome. ROP treatment is commonly done with a special ROP laser under topical anaesthesia (eye drops) by a specialist, where the part of the retina which has not received blood supply is treated. Over 90% of babies respond well to laser treatment and the ROP regresses and vision is preserved. Other than laser, injections into the eye (intravitreal) of a drug that can reverse the abnormal vessel growth are also used in certain conditions. Many of the babies who receive injections will also require laser later. Advanced stages of 4 and 5 will require retinal surgery under general anaesthesia and NICU support.
If treatment is not given on time, the child can become blind or severely visually impaired in both eyes permanently
Narayana Nethralaya is equipped to perform ROP treatments of all forms with ease in new-borns and young children thanks to a dedicated, state of art Paediatric eye surgery operating room. The KIDROP program was the first in the country to use wide-field imaging for ROP screening, which is now considered the new gold standard for ROP screening across the country and has been approved by the national ROP screening guidelines.
If your child had a premature birth(born more than 12 weeks early) and/or had a low birth weight (less than 2 kgs) and has not been screened for ROP in the NICU, you should schedule an appointment with our paediatric retina specialist to get the infant’s eyes checked immediately. Your initial consultation with the doctor will approximately take 2 hours if you do not require cross-consultation and up to 4 hours if you require cross-consultation. During your consultation, our doctors and counsellors will determine the best course of action for your infant’s visual needs, go over the risks and benefits of treatment, and help you choose the best procedure that is suitable for preserving and improving the child’s vision.
Retinopathy of Prematurity (ROP) is an eye condition that affects the retina (nerve tissue of the eye) in premature babies born with a low birth weight. In India, babies who are born less than 2000 grams (2 kgs) or 6 weeks before their due date (34 weeks of gestation) are at risk of ROP.
ROP is caused because the blood supply of the retina remains incomplete when a premature baby is born. These blood vessels need to grow after birth, but fall short in about 30-40% of infants and form a thick ‘barrier’. In some cases (about 5-10%) the barrier grows and damages the retina permanently. Other than premature birth many other factors place these babies at higher risk of ROP, some of them are prolonged use of oxygen, sepsis (blood infection), blood transfusion, jaundice, low weight gain, low platelets, anaemia (low haemoglobin), intraventricular haemorrhage (bleeding in the brain) and many others.
Approximately, 4 out of 10 babies born premature will develop ROP. The other 60% develop their retinal blood vessels spontaneously without any intervention. Of the 40% with disease, nearly 5-10% will develop severe disease that needs treatment to ‘break the barrier’. If the treatment is not given on time, the entire retina gets damaged (retinal detachment) and the child becomes blind or severely visually impaired in both eyes permanently.
Unfortunately, there are no visible signs externally in the early stages of ROP. Due to this, many parents do not get their babies screened on time. In advanced stages there is a white reflex (‘leukocoria’) in the centre of the pupil (round black portion of the eye). Unfortunately, by the time there are signs, it is too late to save useful vision. An untreated infant with advanced ROP will have poor vision, poor eye contact with the parent, abnormal shaking of the eyes (nystagmus) and often delayed milestones as well.
ROP has five stages. To stage these eyes the barrier is assessed. A thin barrier is Stage 1. Stage 2 is diagnosed when the barrier thickens in height and width. Stage 3 is a critical stage, when there are abnormal blood vessels and tissue growing on the barrier and out of it causing bleeding and leakage. Stage 4 is when the barrier increases and lifts the retina from its normal position (detachment) first in the edge (retinal periphery) and then in the visual centre (macula). Stage 5 occurs when the retina is totally detached. Another form of severe ROP is the ‘Aggressive ROP’ (called AROP) where stages 1 to 3 are skipped and it goes directly to stage 4 and 5. These are the most difficult to diagnose and treat.
Most cases with ROP will NOT result in blindness. If the diagnosis is made on time and those that require treatment are identified and treated on time, over 90-95% of babies do very well. APROP has less success and depends on the many factors. The success after treatment of stage 5 ROP are poor even after surgery and case selection and timing of surgery are important.
In India, the national ROP guidelines (2018) recommends that all babies born less than 2000 grams and/or premature less than 34 weeks of gestation, must undergo their first ROP screening before they are 30 days old. The follow-up after that will be determined depending on the findings of the first visit. On an average, a baby will require 3-5 visits to be declared ‘free from ROP’ assuming the baby never develops any disease in any session. These sessions are usually 1-3 weeks apart. If a baby is diagnosed to require treatment (ROP stage 3, ROP stage 2 with plus, AROP) then it must be done within 48 hours for the best outcome.
ROP needs to be diagnosed by an ophthalmologist who is trained in ROP management. The retina of the babies must be visualized after using eye drops that make the pupil bigger (dilatation). Traditionally, an instrument called indirect ophthalmoscope was used by the specialist who would examine and draw the findings on paper. The new alternative is to use retinal photos taken using special (wide-field, contact, infant) cameras which act as a objective report. The Indian national guidelines (2018) formally allowed imaging as the alternative method for ROP screening. These images can be transmitted on a tele-medicine platform or sent to any specialist for an alternate opinion. Images are also useful in explaining to the parents and help in follow-up of the progress of the baby’s condition.
ROP that requires treatment is called ‘Type 1 ROP’ and must be ideally treated within 48 hours of the diagnosis. The ‘gold standard’ for ROP treatment is still laser treatment. This is done by a specialist under topical anaesthesia (eye drop anaesthesia). In laser treatment, the part of the retina which has not received blood supply, (i.e. in front of the barrier) is treated. Other than laser, injections into the eye (intravitreal) of a drug that can reverse the abnormal vessel growth are also used in certain conditions. Many of the babies who receive injections will also require laser later. Advanced stages of 4 and 5 will require retinal surgery under general anaesthesia and may need NICU support.
A very important point to remember is that all premature babies, (even those without ROP) require follow-up even after they are ‘normal’ because they are at a higher risk of low vision, refractive errors (may require to wear glasses even before the first birthday), cortical vision impairment and squint compared to babies born at term (‘9 months’). Since this age is preverbal, special tools and tests are needed to assess vision in these small babies.
“Narayana Nethralaya started the Karnataka Internet Assisted Diagnosis for Retinopathy of Prematurity (KIDROP) program in 2008. Since babies were born in several neonatal intensive care units (NICUs) where there are no ROP specialists to screen and treat on time, KIDROP created a tele-medicine platform on which images taken by mobile teams of trained imagers using specialized ROP cameras, were uploaded and graded by NN’s ROP team.
KIDROP was India’s first tele-ROP program and currently is one of the largest single centre ROP programs in the world. In all, 177 NICUs across the state of Karnataka (Government and Private) are covered each week. Over 321,000 screening sessions have been completed and over 5200 babies treated thus far. This program is a public private partnership with the Government of Karnataka and has mentored other ROP programs across the country. KIDROP has received several awards nationally and internationally for its innovations, including Public Private Partnership of the Year, 2012, National Award for Excellence in HealthCare 2016, K R Datta Award for Community Outreach, 2017 and BIRAC Innovator Award for HealthCare in 2018.”
At Narayana Nethralaya, we are committed to providing our premature infants with advanced quality eye care at affordable prices. These patient experiences stand testimony to the excellence in eye care that we offer.
Narayana Nethralaya
Customer Support
Narayana Nethralaya
Hello, how can I help you today?