Ocular oncology is the speciality dealing with eye tumors. The tumors may stay localised in the eye (Benign) or spread outside (Malignant).
Why should an eye surgeon practice ocular oncology? Aren’t they treated by cancer hospitals?
The eye is a unique structure – treatment of eye tumor has to be done, making sure the tumor is cured; at the same time, as much as possible, the structure and function of the eye is saved. The eye surgeon knows about the eye. The oncologist has knowledge of cancer. The ocular oncologist has knowledge of the eye as well as cancer; thus ocular oncologist is the best choice to plan treatment of an eye cancer. The work is a team effort, including the ocular oncologist, pathologist, medical oncologist for any chemotherapy, and radiation oncologist for radiation therapy

The tumors affecting the white/black part of the eyeball (conjunctiva and cornea)
The eyelid tumors appear as lumps or ulcers (wounds) on the eyelid. When any nodule is removed from the eyelid, a pathology testing is essential to identify whether it is a tumor.
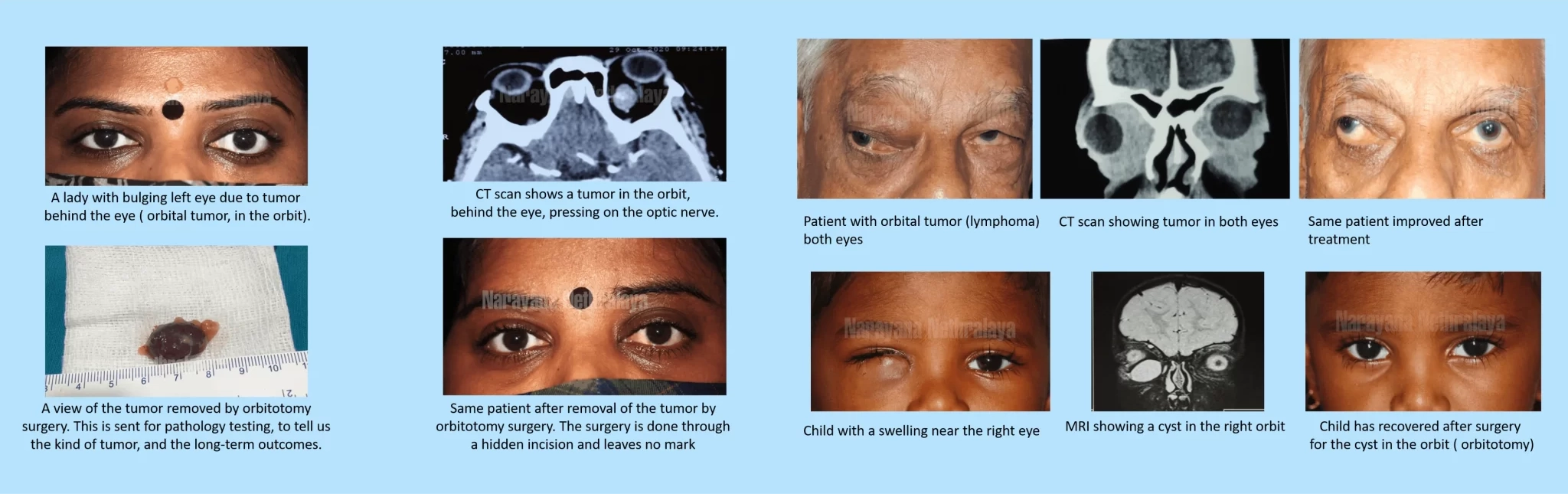
Orbital tumors grow behind the eye, and can cause a bulging eye, double vision, or loss of vision. Usually a CT scan or MRI scan is required to identify presence of a tumor. Only a surgery followed by pathology testing can tell us what kind of tumor it is, and whether further testing and treatment is necessary.
These tumors grow inside the eye, and can present with decreased vision. Retinoblastoma is a life threatening eye cancer that affects children.
Diseases affecting the optic nerve like optic neuritis, ischemic optic neuropathy, autoimmune optic neuropathy, compressive optic neuropathy, nutritional optic neuropathy, toxic optic neuropathy.
characterized by partial of complete inability to move either one or both the eyes due to central and peripheral nervous system diseases like myasthenia gravis and ocular motor cranial nerve palsies following trauma (injury), tumours, ischemia due to systemic diseases like hypertension or diabetes mellitus.
affecting the visual pathway formed by the optic nerve, optic chiasma, optic tract and optic radiations.
like pituitary adenoma, craniopharyngioma, meningioma causing compressive optic neuropathy which cause a direct pressure on the optic nerve and other tumours of the brain affecting the visual pathway and cause of raised intracranial pressure.
such as idiopathic intracranial hypertension, and cerebral venous thrombosis, which can result in permanent and profound loss of vision in the long term
with visual loss, transient ischemic attacks with transient visual loss
We at Narayana Nethralaya believe that no child should be lost to retinoblastoma due to financial constraints. As and when needed, we guide you to sources of monetary support, from government and non – government agencies. Iksha foundation, in particular, gives a stellar contribution towards support of retinoblastoma treatment and works with Narayana Nethralaya.


In some cases, the cancer runs in the family. Genetic analysis can tell us whether a brother or sister of a child is at risk. This information helps to detect the cancer at an earlier stage in other members of the family and can also help parents plan for a future child
From amongst our large database of retinoblastoma patients we can put the parents in touch with other families. The parents are able to share information, and also feel less helpless when they know they are not alone.


It is unfortunate that in our country, people do not know about this life threatening cancer in children. Too often children come to us at an advanced stage because of lack of awareness. We believe this cancer can be detected early and treated only if the collective awareness about the caner increases.
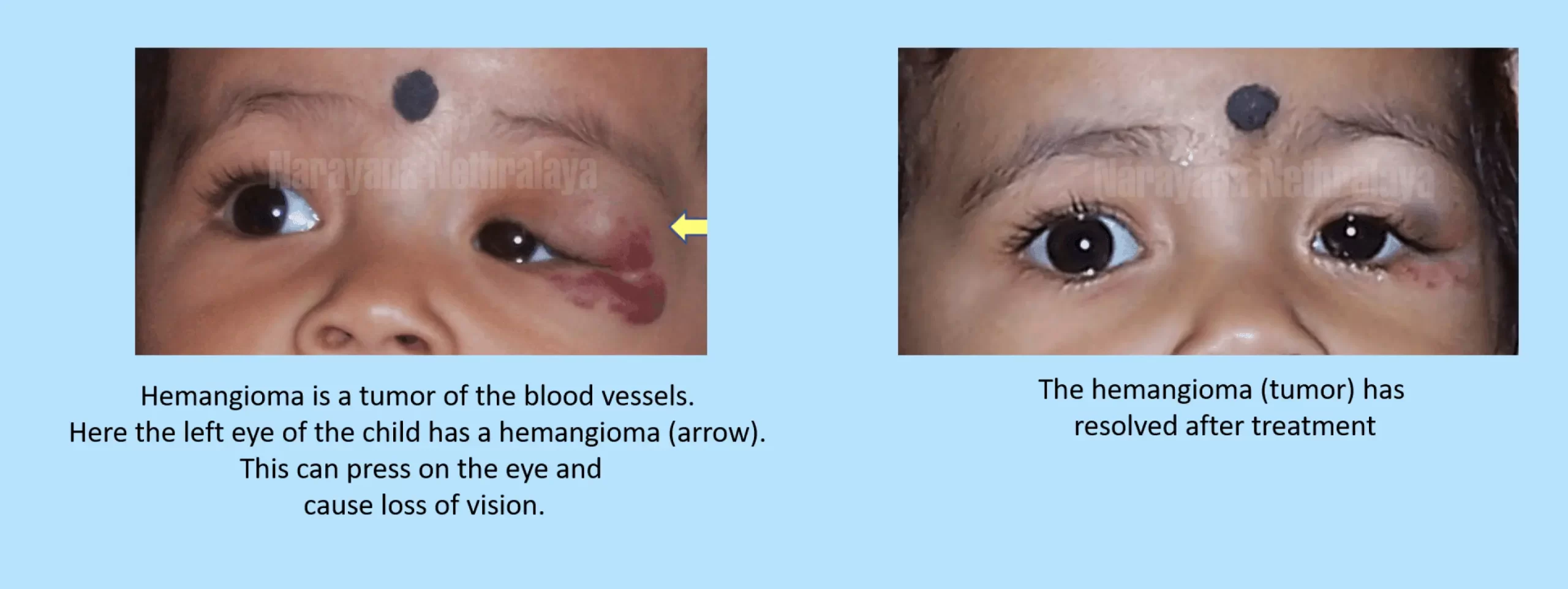
A conjunctival tumor is a growth over the white part of the eye. It may initially appear as a reddish layer growing over the white part of the eye, or a whitish growth over the black part of the eye. It can also be brown or black in colour.
Some conjunctival tumors can be malignant, that is, dangerous. It can spread over the black part of the eye, and even grow inside the eye, thereby endangering the vision.
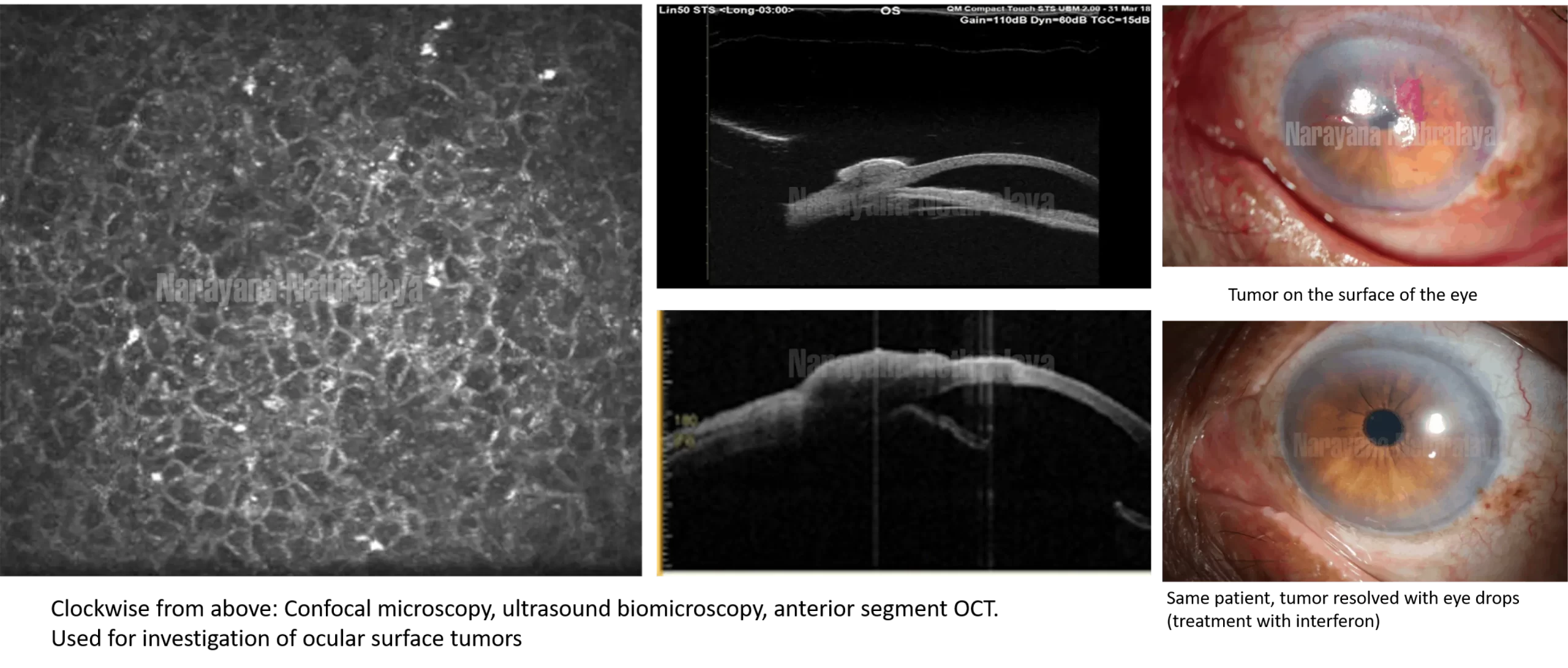
Most tumors are identified during examination by the ocular oncologist. A coloured dye can be applied to the eye to further identify the tumor ( Rose Bengal or Lissamine Green). The tumor is photographed in high resolution using slit lamp photography, so that its progress can be checked. UBM (Ultrasound biomicroscopy) and anterior segment OCT are performed to check whether the tumor is only on the outer surface of the eye, or is it starting to extend inside.
The commonest treatment for a conjunctival tumor is a surgery by minimal-touch technique. The tumor is removed using a delicate surgical process. The tissue around the tumor is treated with cryotherapy ( freezing therapy using liquid nitrous oxide) to prevent spread of the tumor.
Some non-surgical techniques of treatment of conjunctival tumors are –
Freezing therapy (cryo therapy).
Eyedrops – eye drops are mixed in the department from specific injections such as interferon alpha 2 B, mitomycin C, and 5 Fluoro uracil. The term for this treatment is ‘topical chemotherapy’. This is particularly useful for tumors covering the black part of the eye or large tumors. The treatment continues for several months, with testing regularly to check for progress.
The gap left behind by the surgery may be filled by amniotic membrane graft. The tumor is then sent for pathology testing. This confirms whether the tumor is dangerous, and whether further treatment is necessary.
Any lump or swelling growing on the eyelid may be an eyelid tumor.
A lump on the eyelid which has remained the same size for several years is unlikely to be dangerous. It may be a ‘benign’ tumor. Any lump which is growing over a few months, bleeding, forming a wound (ulcer) on the surface – is to be looked at with suspicion. It may be a ‘malignant’, that means, it can spread to other parts of the eye, damage to eye, or even spread to other parts of the body.
The main treatment of an eyelid tumor is by surgery. The surgery is to be done very meticulously, and extra tissue removed around the tumor. This tested by histopathology to ensure there is no tumor left behind (tumor free margins). Then the eyelid is reformed by EYELID RECONSTRUCTION techniques.
Eyelid reconstruction is literally creating a new eyelid or part of an eyelid in place of the part that was removed. It involves delicate oculoplastic techniques (plastic surgery around the eye). Sometimes muscle and skin are moved from the surrounding tissue to fill up the gap (flap technique). Sometimes material can be taken from other parts of the body and stitched on to the eyelid; for example, mucous membrane graft from inside the mouth, skin graft from other part of the body.
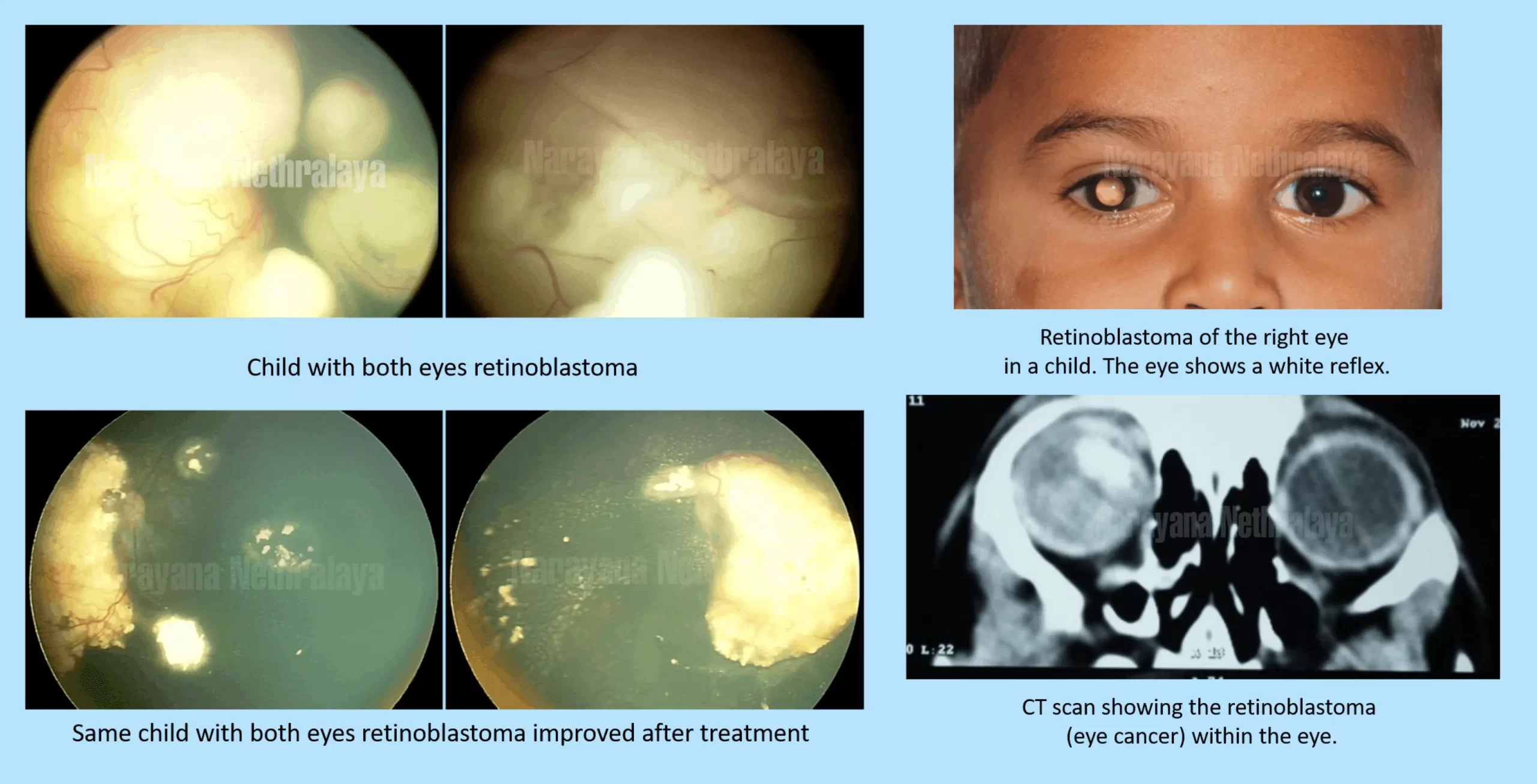
Retinoblastoma is a life threatening eye cancer that affects children. The cancer grows on the sensory layer located inside the eye i.e retina. It is a silent tumour most often detected too late to save the eye.
In early stages the eye looks normal externally. As the cancer progresses it may be observed as a white mass from within the eye. In advance stages, once the cancer spreads outside the eye, it becomes a threat to life.
-White Reflex behind the pupil (leukocoria) – most common
-Squint eyes /crossed eyes
Retinoblastoma is the third most common cancer seen in children occurring 1 in 20000 live births.
Effective treatment is available. 95% of affected children can be saved.
It is treated with a combination of many techniques – surgery, laser, cryo, chemotherapy and radiation.
First, a thorough examination of the eye is done under anaesthesia to know the extent of the disease. In addition, examination of bone marrow and CSF and MRI is done to see if the cancer is only in the eye or whether it has spread elsewhere in the body. Depending on how advanced the cancer is, the doctor may use chemotherapy to shrink the tumour, then apply laser and cryo (freezing therapy). This is done over several sittings till tumour becomes inactive.
Some children may have very advanced disease and the eye has to be removed to save the life. However, with the newest techniques in artificial eye(ocular prosthesis) even such a child can have a near normal appearance. Chemotherapy and radiation may be given in addition, to ensure continued safety of the child.
The doctor always aims to save the life of the child. If the eye can be saved without putting the child in danger, the best efforts are made to save the eye.
Commitment of parents is absolutely crucial for a good outcome. We encourage parents to speak to the doctor about how the treatment is progressing and what the next plan is. Repeated visits for examination (under anaesthesia or in clinic) are very important. Sticking to the schedule of treatment gives the child a much better chance for a favourable outcome.
Finding out their child has cancer is overwhelming for many parents. We have coordinators whose responsibility is to guide the parents through the complex process of staged treatment including scheduling and reminding appointments and guidance for other oncology chemotherapy and MRI appointments.
At Narayana Nethralaya, “Quality of Care” and “Patient Safety” is our priority. Concern for our patients’ well being is at the core of what we do, and what drives us. All 4 units of Narayana Nethralaya are NABH Accredited – the highest national recognition for quality in patient care and safety. Our Oculoplasty team help patients make an informed treatment choice on the type of treatment and surgery that is best suited for their lifestyle. We have an exclusive counseling team to address any doubts or questions that people may have about Oculoplasty treatment options and procedures.
