Cortical Visual Impairment (CVI) Therapy at Buds to Blossoms Clinic
What is Cortical Visual Impairment?
Cortical Visual Impairment (CVI) is a brain-based visual disorder where the eyes may appear structurally normal, but the brain has difficulty processing visual information. CVI is one of the most common causes of visual impairment in children, particularly those with neurological conditions or a history of brain injury.
Despite healthy-looking eyes, a child with CVI may struggle to:
- Recognize objects
- Track movement
- Respond to visual cues
This is because their visual processing system in the brain is impaired.
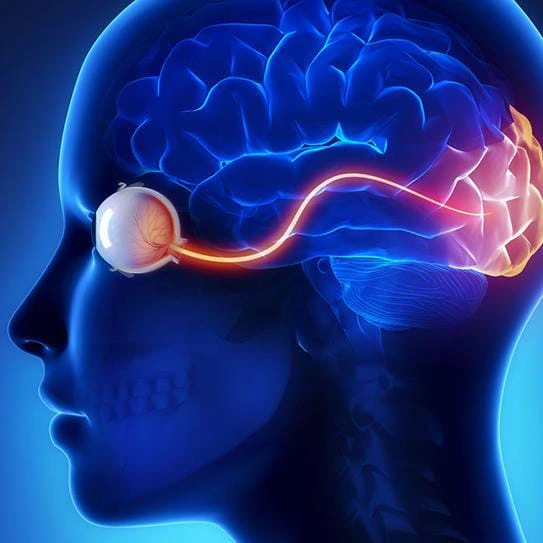
Understanding Vision Beyond the Eyes
Vision is not just about what the eyes see—it’s about how the brain interprets those images.
“Tree of Vision” – Brain Regions Involved:
- Occipital lobe – helps you see
- Temporal lobe – tells you what you're seeing
- Parietal lobe – tells you where it is
In CVI, this process is disrupted, resulting in poor visual perception despite healthy eyes.
Common Causes of CVI
- Birth complications (e.g., low oxygen or glucose levels)
- Severe infections in early infancy
- Traumatic brain injury
- Seizure disorders
- Cerebral palsy
Signs Your Child May Have CVI
- Difficulty walking downstairs but climbs up easily
- Doesn’t notice fast-moving objects (e.g., vehicles, pets)
- Doesn’t respond to distant pointing cues (e.g., moon, bird)
- Trouble locating objects in cluttered environments
- Difficulty copying from the board
- Trouble writing within lines
- Poor hand-eye coordination
Our CVI Assessment & Therapy Approach
Multidisciplinary Assessment at Buds to Blossom
Our comprehensive CVI assessment includes:
- Pediatric Ophthalmologists & Optometrists:
Assess refractive errors, squint, retinal issues
Correct these issues for improved therapy outcomes
- CVI Functional Visual Assessment:
Visual attention and tracking
Visual-motor coordination
Brain imaging (MRI) when needed
- Pediatric Neurologist Evaluation

Integrated CVI Therapy
Step 1: Correction
- Prescription glasses
- Squint correction
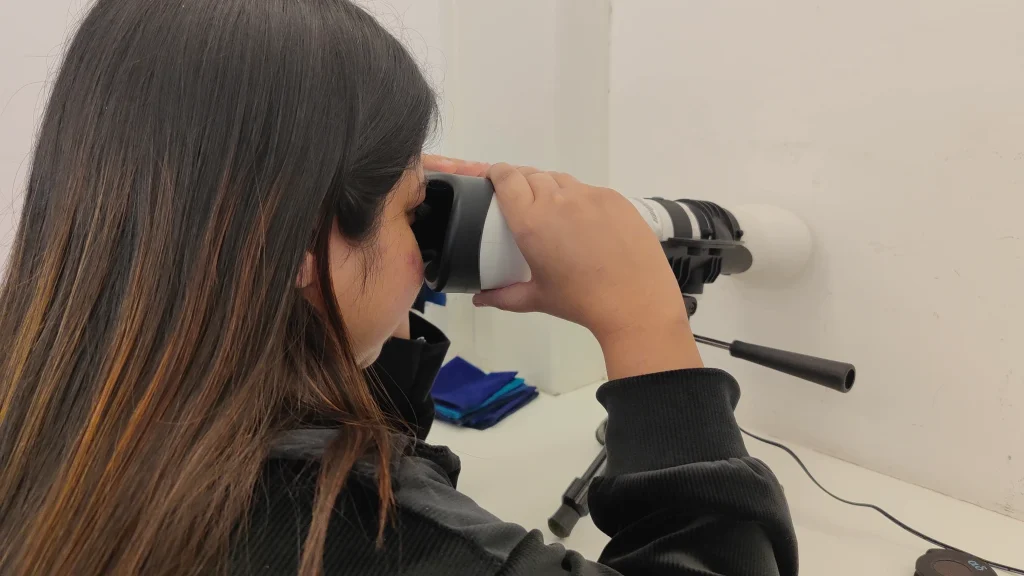
Step 2: Visual Therapy Tools
- Computer-based exercises:
Senaptec Vision Integrator
Vision Therapy System 4
- Marsden Ball therapy
- Marsden with balance board
Step 3: Holistic Development Support
- Physiotherapy
- Occupational therapy
- Speech and language therapy
- Special education support
- Child psychology services
Family Involvement & Long-Term Success
Empowering parents is vital. We offer:
- Parent counseling & training
- Home program guidance
- Regular follow-ups with therapy plan adjustments
Consistency and support at home are key to helping children with CVI thrive.
Let Us Help Your Child See the World Better
If your child shows signs of CVI or has a history of neurological challenges, early intervention is crucial.

Now Eye Know Videos
Frequently Asked Questions
How Much Vision Will a Child with CVI Have?
Vision in CVI varies widely. Some children may appear to see normally, while others have significant difficulties. Importantly, many retain the ability to perceive movement, which can be used in therapy to improve functional vision.
Can CVI Therapy Be Done at Home?
Yes. While advanced therapy requires clinical equipment, home-based activities are essential and improve outcomes when combined with clinic visits.
Will My Child Need Glasses?
If a refractive error or squint is present, glasses may be needed. Sometimes plus-powered glasses are prescribed to improve near vision.
Will My Child Ever Be “Normal”?
CVI is a spectrum, and every child’s abilities and challenges are unique. While some children may have visible physical or neurological differences, the right combination of therapies can help maximize their functional abilities. With ongoing support, many children with CVI can learn to adapt, grow, and achieve their full potential, regardless of the underlying structural challenges.
Can My Child Go to a Regular School?
Yes, if developmental delays are not severe. Many children with CVI successfully attend regular schools, often with additional academic support. At Buds to Blossom, we have a special educator who can work closely with you to assess your child’s learning needs and help implement strategies for better performance in school.
How Long Should Therapy Continue?
The duration of CVI therapy varies depending on several factors, including:
The underlying cause of CVI
The child’s age and stage of development
The rate of progress and response to therapy
Consistency and compliance with therapy sessions
There is no fixed timeline—some children show improvement quickly, while others may need longer. The key is to be patient, consistent, and hopeful. Regular follow-ups help in adjusting the therapy plan as your child progresses.
Is CVI Considered a Disability?
Currently, the Government of India does not recognize CVI as a separate disability. However, children may qualify under broader categories like low vision or motor delays. We assist families with documentation and guidance in this regard.
Vision Rehabilitation: Empowering Independence and Confidence
What is Rehabilitation?
Rehabilitation helps individuals with disabilities regain and maintain optimal daily functioning. It includes:
Our Vision Rehabilitation Department empowers individuals with visual impairment to live independently by focusing on:
- Assistive devices
- Environmental modifications
- Daily activity training
Aims of Rehabilitation
- Prevent or slow functional loss
- Restore lost functions
- Compensate for lost abilities
- Maintain current functionality
What is Vision Rehabilitation?
Our Vision Rehabilitation Department empowers individuals with visual impairment to live independently by focusing on:
- Orientation and mobility training
- Adaptive techniques
- Assistive technology (e.g., Braille, screen readers)
Who Needs Vision Rehabilitation?
- Congenital/acquired vision loss
- Progressive vision loss
- Low vision (acuity below 6/18)
- Neurological impairments (e.g., CVI)
- Developmental or motor delays
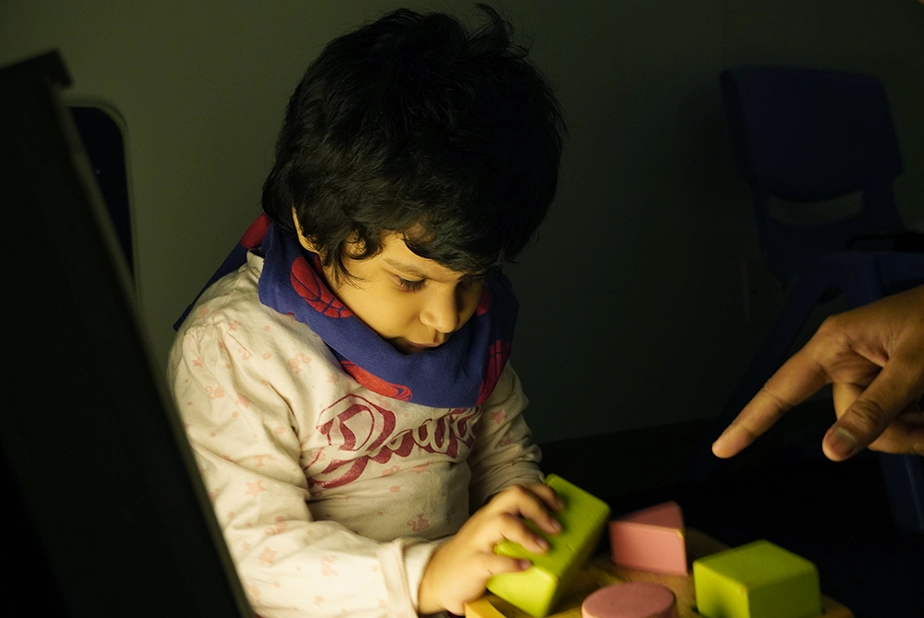
Benefits for Children
- Functional vision evaluation
- Visual stimulation
- Early intervention (birth–6 years)
- Improved motor, cognitive, language, and play skills
Types of Rehabilitation
Process of Rehabilitation Services
Early Intervention
History
- Collecting demographic details (basic details)
- Prenatal, birth, and postnatal history
- Medical history (MRI, EEG, BERA, etc.)
- Family history
Holistic Assessment
Functional Vision Assessment
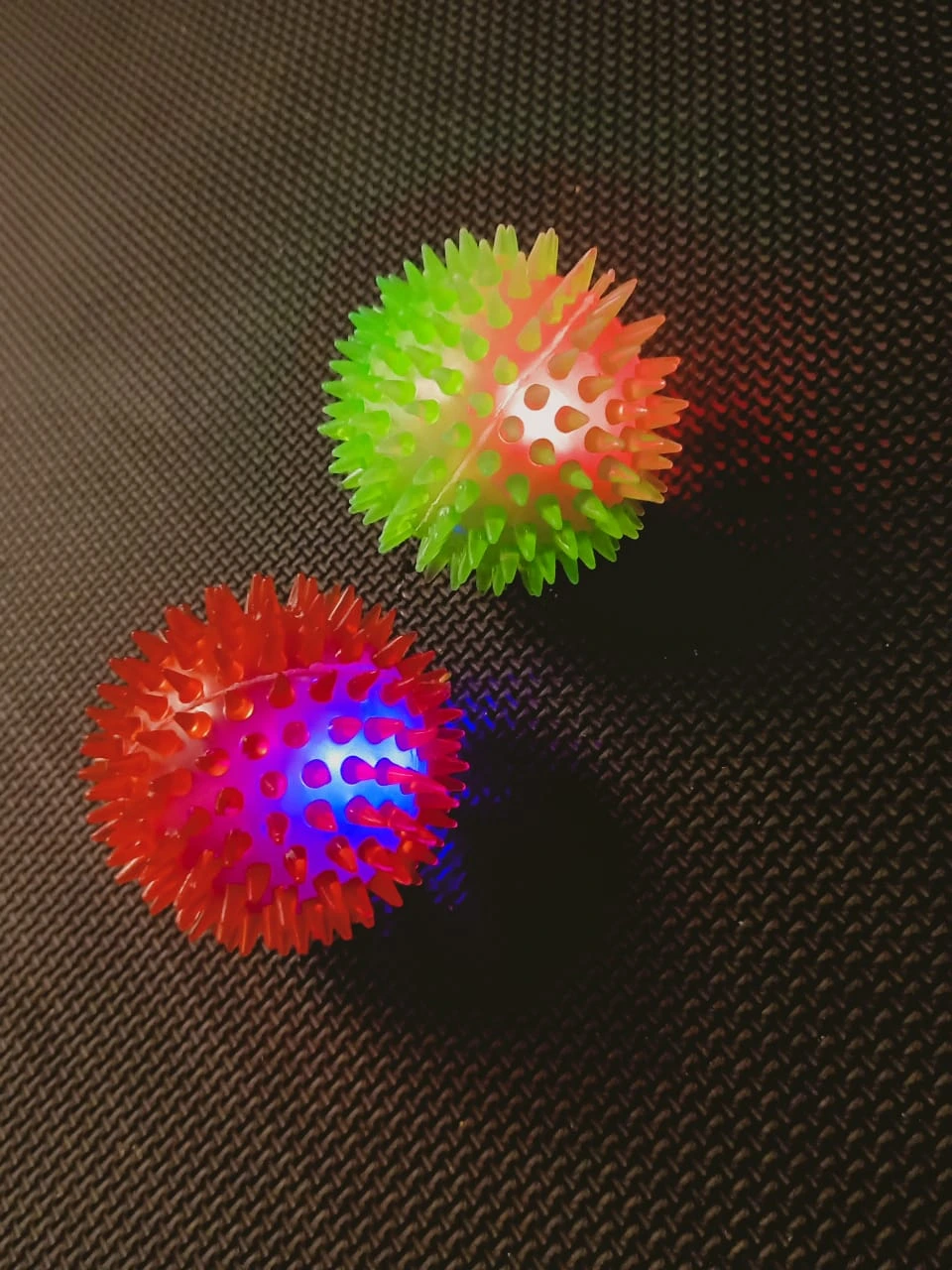
- e.g., glow balls, eye-hand coordination
Functional Developmental Assessment
- Auditory
- Tactile
- Gross motor
- Fine motor
- Receptive communication
- Expressive communication
Behavioural Assessment
- Observation of mannerisms
Child Rehabilitation
History
- Educational history
- Performance of the child – reading, writing, arithmetic
- Understanding and delivering concepts
- Storing and retrieving concepts from memory
Comprehensive Assessment
- Vision Assessment – Near and distance vision, colour, contrast
- Eye-hand coordination
- Orientation
- Finger dexterity
- Reading – errors, difficulties, posture, pace of reading
- Writing – posture, legibility, pressure in writing, spacing in writing
- Attention – interest-based, sustained attention
- Behavioural analysis – sitting tolerance, non-disruptive behaviour
Visual Processing
- Visual memory
- Visual-spatial orientation
- Figure-ground discrimination
- Visual closure
- Visual sequencing
- Depth perception
- Auditory processing – auditory memory, comprehension, retrieval
- Communication – comprehension, clarity, fluency
- Social interaction and contribution
- Community orientation and participation
- Sensory sensitivity – visual (vision), auditory (hearing), olfactory (smell), gustatory (taste), tactile (touch)
- Activities of Daily Living (ADL) – independent or non-independent
Motor Coordination and Balance

Intervention Procedures and Therapies

Vision Stimulation Exercises
- Rope light stimulation
- Stimulation with shiny materials and glow balls/toys
- Stimulation with pattern charts and bright coloured toys
- Fixation, pursuits, and saccades
- Eye contact
- Face recognition
Sensory Integration Therapy
- Auditory stimulation with varying frequencies
- Olfactory stimulation with varying fragrances
- Gustatory stimulation with varying tastes
- Tactile stimulation with different textures
Communication
- Face-to-face interaction
- Description of activities
- Blowing activities
- Sound production
- Single words, two-word phrases, sentence communication

Gross Motor Coordination
- Range of motion (ROM) exercises
- Strengthening exercises
- Home-based activities targeting areas of delay
Finger Dexterity
- Holding rattles and toys
- Kneading activities (e.g., playing with dough)
- Free finger movements (e.g., water splash)

Eye-Hand Coordination with Cognitive Involvement
- Single and double-handed activities (e.g., threading beads, stacking rings, connecting links)

Concept Awareness
- Concepts such as body parts, everyday objects, colours, fruits, vegetables, animals, transport, etc.
- Understanding concepts of big/small, more/less weight, etc.
Pre-Reading Skills
- Picture comprehension
- Rhyming
- Matching, sorting, numbering
- Letter recognition, direction
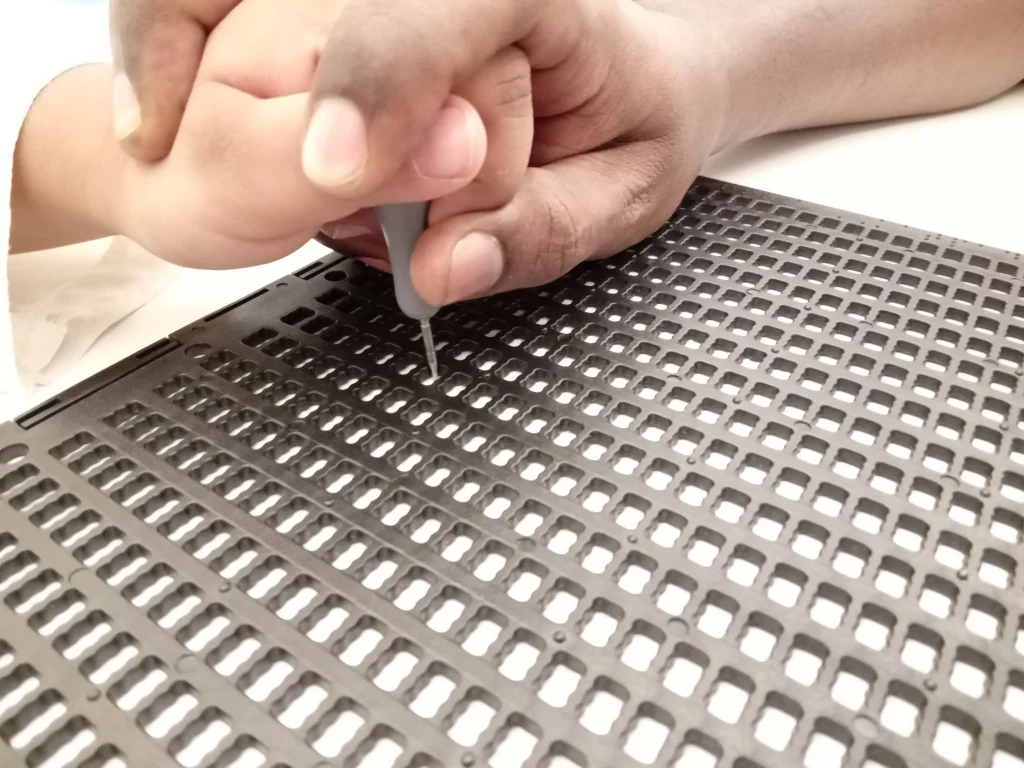
Pre-Writing Skills
- Printing activities
- Scribbling, colouring, connecting dots, etc.
Reading Training
- Syllabification
- Tracking the finger while reading
- Word scanning
- Improving reading pace through rehearsals
Writing Training
- Using bold-lined notebooks and dark pencils
- Correct posture and pencil grip
- Maintaining appropriate spacing in writing
Environmental Modifications
- Adjustments in lighting, seating, tables, etc.
We Treat
- Visually impaired (total/partial blindness)
- Intellectual disability
- Physical impairment (e.g., cerebral palsy)
- Speech impairments
- Autism and ADHD
- Learning disability
Download Rehabilitation Skill Training Brochure
Adult Rehabilitation
Assessment Areas
- Visual prognosis
- Reading/writing
- Orientation and mobility
- ADL independence
- Job satisfaction and support needs
- Psychological and social support
Counseling:
- Individual and family counseling
- Awareness of rights and government schemes
Support Available
- Disability certificate (UDID)
- Monthly pension
- Transportation concessions
- Job reservations

Adult Rehabilitation
Assessment Areas
- Visual prognosis
- Reading/writing
- Orientation and mobility
- ADL independence
- Job satisfaction and support needs
- Psychological and social support
Counseling:
- Individual and family counseling
- Awareness of rights and government schemes
Support Available
- Disability certificate (UDID)
- Monthly pension
- Transportation concessions
- Job reservations
Adjunctive Therapy and Rehabilitation Services
Physiotherapy
Empowering Children Through Movement
Our Pediatric Physiotherapy Department is dedicated to supporting children with physical disabilities or motor challenges to achieve their full potential. We work closely with children and their families to create personalized treatment plans that foster:
- Physical development
- Improved mobility
- Greater independence

Therapeutic Exercises for Physical Growth
Our sessions are designed to be fun, engaging, and age-appropriate, using play-based approaches to help children:
- Develop gross motor skills
- Enhance balance and coordination
- Build muscle strength and endurance
- Improve posture and movement control
These therapeutic exercises allow children to fully participate in daily activities, school, and play, boosting their confidence and overall quality of life.
Our Goals
- Help children overcome physical challenges
- Support the achievement of key developmental milestones
- Promote long-term physical wellness through early intervention
If your child is facing challenges in movement or physical development, our dedicated physiotherapy team is here to help them move, grow, and thrive.
Occupational Therapy
Our Occupational Therapy Department helps children develop the skills they need to participate fully in daily activities and achieve independence.

Focus Areas
- Fine motor skill development
- Sensory integration
- Cognitive abilities enhancement
These skills empower children to engage in:
- Play
- Self-care
- Educational activities with confidence
Play-Based Interventions for Skill Development
Using play-based therapy and individualized treatment plans, we help children overcome functional challenges and unlock their full potential—enhancing their overall quality of life.
Special Education
Our Special Education Department is committed to providing inclusive, high-quality education to children with disabilities.
Our Goals
- Improve academic outcomes
- Ensure equal access to education
- Support learning irrespective of ability or background
Creating Inclusive Education for All
We collaborate with families, educators, and support professionals to build a system that adapts to the learner’s needs, promoting equity, participation, and success for all students.

Speech Therapy
The Speech Therapy Department supports individuals with communication and oral-motor challenges.

Conditions We Address
- Articulation disorders
- Language delays
- Stuttering
- Feeding and swallowing difficulties
Improving Communication and Oral Skills
Through personalized sessions, we offer:
- Oromotor therapy
- Language and speech development
- Enhanced ability to express needs, emotions, and ideas confidently
Cognitive Therapy
Our Cognitive Therapy Department helps individuals facing:
- Memory loss
- Attention deficits
- General cognitive impairments
Enhancing Cognitive Function and Independence
With tailored strategies and structured interventions, we support patients in:
- Improving memory and attention
- Boosting cognitive skills
- Gaining greater independence and quality of life
Advanced Tools and Technology
Syntonic Phototherapy
A non-invasive light therapy designed to stimulate the brain and nervous system for therapeutic benefits.
Benefits
- Improved visual processing
- Reduced stress
- Enhanced relaxation and brain function
Therapeutic Light for Neurological Health
We use specific wavelengths of light to promote neurological health.
This innovative approach is designed to enhance brain function, mental clarity, and reduce stress, providing patients with a sense of comfort and relaxation.
It can also be used in Traumatic Brain Injury (TBI) and Brain Stroke to stimulate the brain and nervous system. This therapy helps improve neurological function, reduce symptoms like headaches and light sensitivity, and supports overall recovery. It is a non-invasive approach that promotes better brain balance and healing.
Elisar Advanced Vision Analyzer (AVA)
Our department is equipped with this state-of-the-art tool for visual field assessments.
Key Features
- Precise diagnosis of visual field defects
- Accurate monitoring of treatment progress
- Supports management of neurological and ocular conditions
The Elisar AVA ensures patients receive comprehensive, data-driven care for optimal visual outcomes.

Conditions We Address
Prism Trial Therapy
We offer customized prism therapy solutions for patients with:
- Diplopia (double vision)
- Visual field loss
- Other binocular vision impairments
Prism Options
Through personalized sessions, we offer:
- Press-On Peli Prisms
- Fresnel Prisms
- Yoke Prisms
Our expert team evaluates each case to find the most effective prism solution, improving:
- Visual alignment
- Depth perception
- Overall visual comfort